Interview: The nuts and bolts of blood flow
 Amanda Randles is the Alfred Winborne and Victoria Stover Mordecai associate professor of biomedical sciences at Duke University. She developed HARVEY, a novel model for simulating blood flow during her Harvard University Ph.D. research, where she was a Department of Energy Computational Science Graduate Fellowship (DOE CSGF) recipient, with Efthimios Kaxiras and Hanspeter Pfister. Her Duke team continues to improve and expand the model’s biomedical uses, which include building digital twins, or computational copies, of patients’ circulatory systems and studying how metastasizing cancer cells travel through the bloodstream. She was one of the inaugural winners of the Sony Women in Technology Award with Nature in 2025 and has garnered numerous other honors, including a 2024 ISC Jack Dongarra Early Career Award and the 2023 ACM Prize in Computing. This interview has been edited for clarity and length. It is reprinted here from the 2025 print issue of DEIXIS: The DOE CSGF Annual.
Amanda Randles is the Alfred Winborne and Victoria Stover Mordecai associate professor of biomedical sciences at Duke University. She developed HARVEY, a novel model for simulating blood flow during her Harvard University Ph.D. research, where she was a Department of Energy Computational Science Graduate Fellowship (DOE CSGF) recipient, with Efthimios Kaxiras and Hanspeter Pfister. Her Duke team continues to improve and expand the model’s biomedical uses, which include building digital twins, or computational copies, of patients’ circulatory systems and studying how metastasizing cancer cells travel through the bloodstream. She was one of the inaugural winners of the Sony Women in Technology Award with Nature in 2025 and has garnered numerous other honors, including a 2024 ISC Jack Dongarra Early Career Award and the 2023 ACM Prize in Computing. This interview has been edited for clarity and length. It is reprinted here from the 2025 print issue of DEIXIS: The DOE CSGF Annual.
DEIXIS: YOUR TRAINING IS IN COMPUTER SCIENCE AND PHYSICS, BUT YOUR RESEARCH FOCUSES ON BIOLOGY AND MEDICINE. HOW DID YOU GET INTERESTED IN THIS INTERSECTION?
 Amanda Randles: In high school, I learned to program and got excited about important biological questions. But I liked understanding the nuts and bolts of how things work.
Amanda Randles: In high school, I learned to program and got excited about important biological questions. But I liked understanding the nuts and bolts of how things work.
So as an undergraduate at Duke University, I knew I wanted to study physics. The Human Genome Project had just come out, and I was interested in how science affected policy. So I was planning to add a second major in political science or international relations. But while helping friends with some of their coding classes, I realized how much I missed computer science. I ultimately had a double major in computer science and physics with a minor in political science.
As part of a biotechnology program at Duke, I visited both the Craig Venter Institute and an NIH lab. They were collecting so much data but had to figure out how to analyze it. It became clear how much computer science could help answer biological questions, and I was excited.
After graduation, I was offered a dream job at IBM on the Blue Gene supercomputer, where they were studying biomedical problems at a scale that you couldn’t do otherwise. That was my first experience with parallel computing, and it led me back to graduate school and to using supercomputers and physics principles to study biological questions.
WHAT QUESTIONS ARE YOU FOCUSING ON NOW?
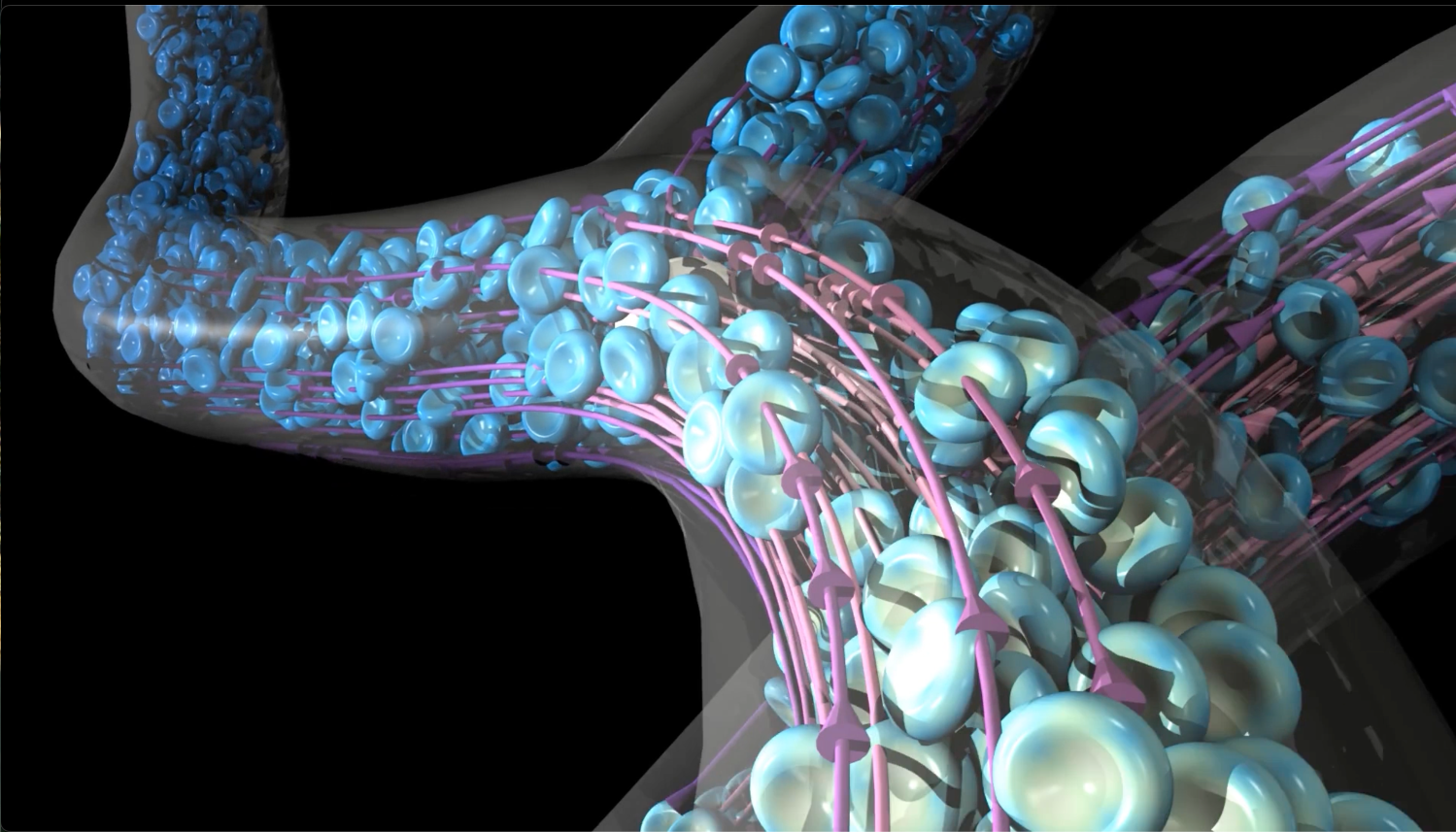
We’re still using HARVEY to create patient-specific, 3D bloodflow simulations and even digital twins of specific patients.
When cardiologists evaluate whether they need to place a stent, they’ve traditionally measured the pressure gradient in the blood vessel by running a guidewire inside the artery. We developed this computational tool so you can make a 3D model of the patient’s heart, run a blood-flow simulation and measure the pressure gradient in that 3D virtual model.
In a clinical trial with 200 patients, we showed that this computational measurement, called the fractional flow reserve, was accurate and can determine noninvasively if the patient needs a stent.
Now we’re interested in connecting these blood-flow simulations to wearable devices so that we can monitor patients over months to identify when someone’s going to have an issue before it happens, like a check-engine light for the heart, that could help a doctor act proactively and bring a patient in for further tests.
There are a lot of computational challenges. Previously, it took the world’s biggest supercomputer just to model a single heartbeat. We’ve moved from the previous modeling record, about 30 heartbeats, to six weeks’ worth — about 4.5 million heartbeats.
And then on the other end, we want to examine individual cells to understand why a cancer cell interacts with the vessel wall. We’ve added adhesion models to simulate individual ligand receptors on a cancer cell adhering at different locations in the body.
YOU WERE AN EARLY USER OF ARGONNE’S EXASCALE COMPUTER AURORA. WHAT HAVE YOU DONE SO FAR?
Back in 2010, it took Argonne’s biggest supercomputer, around 140,000 processors, six hours just to run one heartbeat with high resolution to understand the flow patterns in coronary arteries. In 2015, with Livermore’s system, we went to the fullbody level but only modeling vessels a millimeter in diameter or above.
Now with Aurora, we can run that full-body simulation on a smaller portion of the system, which really allows us to run many simulations and do more exploratory science. We can vary the heart rate or other characteristics known to be linked with disease development.
With digital twins, where we’re trying to capture six months, we need tons of compute. As we look at the cellular components with Aurora, we’ve been able to model at least a few billion red blood cells.
That’s only a small fraction of the red blood cells in your body, but it’s a huge amount to really understand how a cancer cell might be moving and where it’s interacting with the red blood cells. These simulations produce terabytes to petabytes of data.
These days we’re doing in situ visualizations while everything is still in memory on Aurora because you can’t really download a petabyte of data, take it to another system and try to visualize it there.
YOU HAVE A LARGE MEDIA FOOTPRINT AND PARTICIPATE IN POLICY DISCUSSIONS. WHY?
AI and digital twins are important subjects for the public to understand, and people want to hear directly from the experts. How are we using it? How is this really going to help you? And what’s the difference between science fiction and the tangible?
With wearables, for example, patients now have access to their own medical information, unlike when all medical records stayed with doctors. It’s important for the patient to really understand those opportunities.
DOE’s Exascale Computing Project really helped us move forward technology, not just hardware but also software and workforce training. We need to have a clearer plan of what follows, so we need to talk about maintaining and improving those gains intelligently. It’s an important conversation to be having with policymakers and with the public.
HOW HAS THE DOE CSGF INFLUENCED YOUR CAREER?
Aside from the original funding that made HARVEY possible, the DOE CSGF set up important interactions. I did a practicum and then I was a Lawrence Fellow at Lawrence Livermore National Laboratory.
I had many mentors through the program that helped me figure out the next stage of my career. Even now, I go to people like David Keyes and ask him for career advice. It’s a network outside your graduate program that creates a personal and professional community. At Duke, we’ve been setting up a virtual seminar series on computational and digital health, and a variety of former DOE CSGF fellows have been speakers.
WHAT ADVICE WOULD YOU GIVE TO EARLY CAREER RESEARCHERS?
Be comfortable, especially within a community like the DOE CSGF, to ask for advice. Don’t be offended if people don’t respond, but it’s okay to reach out and ask for informational interviews and other help.
On the research front, think about what really motivates you. Be willing to take big risks and try crazy projects. Many interesting things can come out of interdiscip
About the Author
Sarah Webb is science communications manager at the Krell Institute. She’s managing editor of DEIXIS: The DOE CSGF Annual and producer-host of the podcast Science in Parallel. She holds a Ph.D. in chemistry, a bachelor’s degree in German and completed a Fulbright fellowship doing organic chemistry research in Germany.





You must be logged in to post a comment.